Diabetes is a chronic metabolic disorder characterized by elevated blood glucose levels due to the body’s inability to produce or effectively use insulin. Insulin is a hormone produced by the pancreas that regulates blood sugar. Without proper management, diabetes can lead to severe complications affecting various organs. This article explores the causes, symptoms, prevention, diagnosis, and treatment of diabetes.
Types of Diabetes
Diabetes is categorized into several types, each with distinct causes and characteristics:
1. Type 1 Diabetes
- An autoimmune condition in which the immune system attacks insulin-producing beta cells in the pancreas.
- Typically develops in childhood or adolescence but can occur at any age.
- Patients require daily insulin therapy.
2. Type 2 Diabetes
- The most common form of diabetes, characterized by insulin resistance and eventual insulin deficiency.
- Often associated with lifestyle factors such as obesity, inactivity, and poor diet.
- Can develop at any age, but more common in adults.
3. Gestational Diabetes
- Occurs during pregnancy when hormonal changes impair insulin function.
- Typically resolves after delivery but increases the risk of developing type 2 diabetes later.
4. Other Specific Types
- Includes monogenic diabetes (caused by genetic mutations) and diabetes secondary to medical conditions or medications.
Causes of Diabetes
The causes of diabetes vary depending on its type:
Type 1 Diabetes
- Caused by an autoimmune response that destroys insulin-producing cells.
- Exact triggers are unclear but may include genetic predisposition and environmental factors such as viral infections.
Type 2 Diabetes
- Results from a combination of genetic and lifestyle factors, including:
- Obesity and physical inactivity.
- Family history of diabetes.
- Unhealthy diet high in refined carbohydrates and sugars.
- Chronic stress or poor sleep.
Gestational Diabetes
- Caused by hormonal changes during pregnancy that reduce insulin sensitivity.
- Risk factors include obesity, advanced maternal age, and a history of gestational diabetes in previous pregnancies.
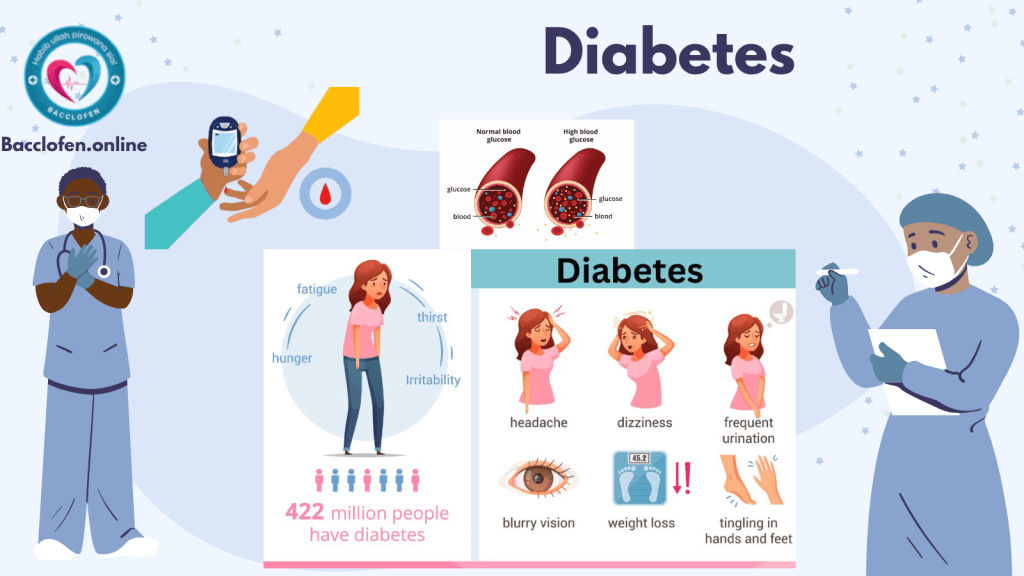
Symptoms of Diabetes
Symptoms of diabetes can vary in intensity and may develop gradually, especially in type 2 diabetes.
Common Symptoms
- Frequent urination (polyuria).
- Excessive thirst (polydipsia).
- Unexplained weight loss.
- Extreme hunger (polyphagia).
- Fatigue and irritability.
- Blurred vision.
- Slow-healing wounds or frequent infections.
Advanced Symptoms
- Numbness or tingling in the hands and feet (neuropathy).
- Darkened skin patches, particularly around the neck or armpits (acanthosis nigricans).
Complications of Diabetes
Without effective management, diabetes can lead to severe, long-term complications, including:
- Cardiovascular Disease: Increased risk of heart attacks, strokes, and hypertension.
- Kidney Damage (Nephropathy): Diabetes is a leading cause of chronic kidney disease and failure.
- Eye Damage (Retinopathy): High blood sugar can damage the retina, potentially causing blindness.
- Nerve Damage (Neuropathy): Can result in pain, numbness, or loss of function in the extremities.
- Foot Problems: Poor circulation and neuropathy increase the risk of ulcers and infections, potentially leading to amputations.
Prevention of Diabetes
While type 1 diabetes cannot be prevented, steps can be taken to reduce the risk of type 2 and gestational diabetes.
1. Maintain a Healthy Diet
- Emphasize whole grains, lean proteins, fruits, and vegetables.
- Avoid sugary drinks and processed foods high in trans fats and refined sugars.
2. Regular Physical Activity
- Engage in at least 150 minutes of moderate exercise weekly, such as walking, swimming, or cycling.
- Strength training improves insulin sensitivity and overall metabolic health.
3. Maintain a Healthy Weight
- Achieving and sustaining a healthy weight reduces the risk of type 2 diabetes.
4. Manage Stress
- Chronic stress can raise blood sugar levels. Practices such as meditation, yoga, and deep breathing can help.
5. Regular Monitoring
- Individuals with risk factors, such as a family history of diabetes, should monitor blood sugar levels regularly and consult healthcare providers for early interventions.
Diagnosis of Diabetes
Several tests can confirm a diabetes diagnosis, including:
1. Fasting Blood Glucose Test
- Measures blood sugar after fasting for at least eight hours. A level of 126 mg/dL or higher indicates diabetes.
2. Oral Glucose Tolerance Test (OGTT)
- Measures blood sugar before and two hours after consuming a sugary drink.
3. Hemoglobin A1c Test
- Reflects average blood sugar levels over the past two to three months. An A1c level of 6.5% or higher indicates diabetes.
4. Random Blood Glucose Test
- A random blood sugar level of 200 mg/dL or higher, along with symptoms, confirms diabetes.
5. Gestational Diabetes Testing
- Screening between 24 and 28 weeks of pregnancy using OGTT.
Treatment of Diabetes
Effective diabetes management involves a combination of lifestyle modifications, medications, and monitoring.
1. Lifestyle Changes
- Dietary Management: Work with a dietitian to develop a balanced eating plan that stabilizes blood sugar.
- Exercise: Regular physical activity enhances insulin sensitivity and helps control blood sugar.
2. Medications
- Insulin Therapy: Essential for type 1 diabetes and sometimes for type 2 diabetes.
- Oral Medications:
- Metformin improves insulin sensitivity and reduces glucose production in the liver.
- Sulfonylureas and meglitinides stimulate insulin production.
- Injectable Medications: GLP-1 receptor agonists help regulate blood sugar and support weight loss.
3. Blood Sugar Monitoring
- Regular glucose monitoring using glucometers or continuous glucose monitors (CGMs) helps patients maintain optimal control.
4. Advanced Therapies
- Artificial Pancreas Systems: Combines CGMs with insulin pumps for automated blood sugar control.
- Bariatric Surgery: Effective for managing type 2 diabetes in obese patients.
Living with Diabetes
Managing diabetes requires commitment and consistent care. With proper management, individuals with diabetes can lead healthy and active lives.
Tips for Effective Management
- Adhere to Treatment Plans: Follow medication schedules and dietary recommendations.
- Regular Health Checkups: Monitor for complications such as eye, kidney, and cardiovascular issues.
- Stay Educated: Stay informed about diabetes and advancements in treatment.
Research and Future Directions
Advances in diabetes research hold promise for improving treatment and potentially finding a cure:
- Artificial Intelligence in Diabetes Care: AI tools are being developed for personalized treatment plans.
- Stem Cell Therapy: Research into stem cells aims to regenerate insulin-producing beta cells.
- Gene Editing: Techniques like CRISPR are being explored to correct genetic mutations causing diabetes.
Also check
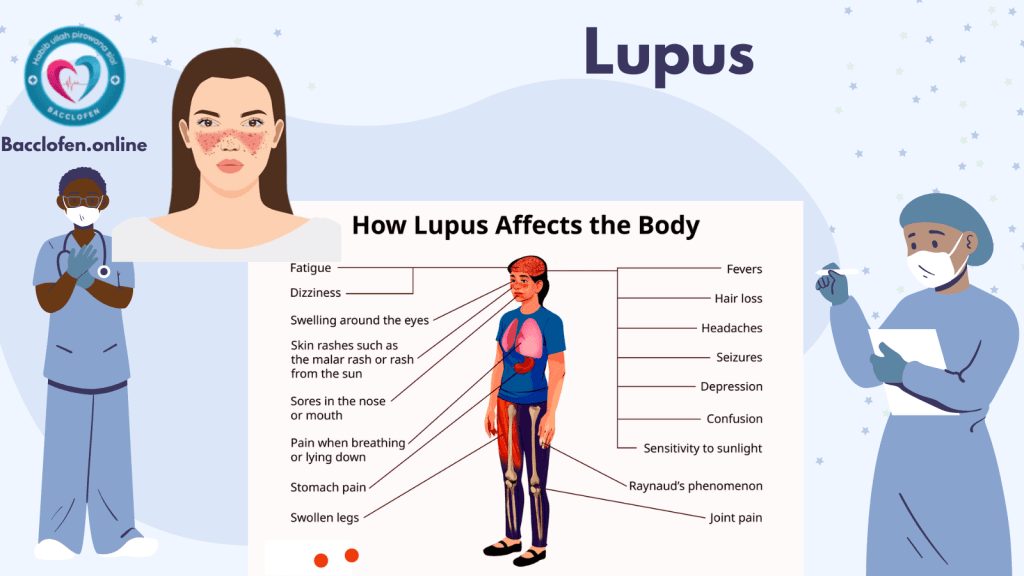
Pingback: Lupus: Causes, Symptoms and Treatment - Bacclofen