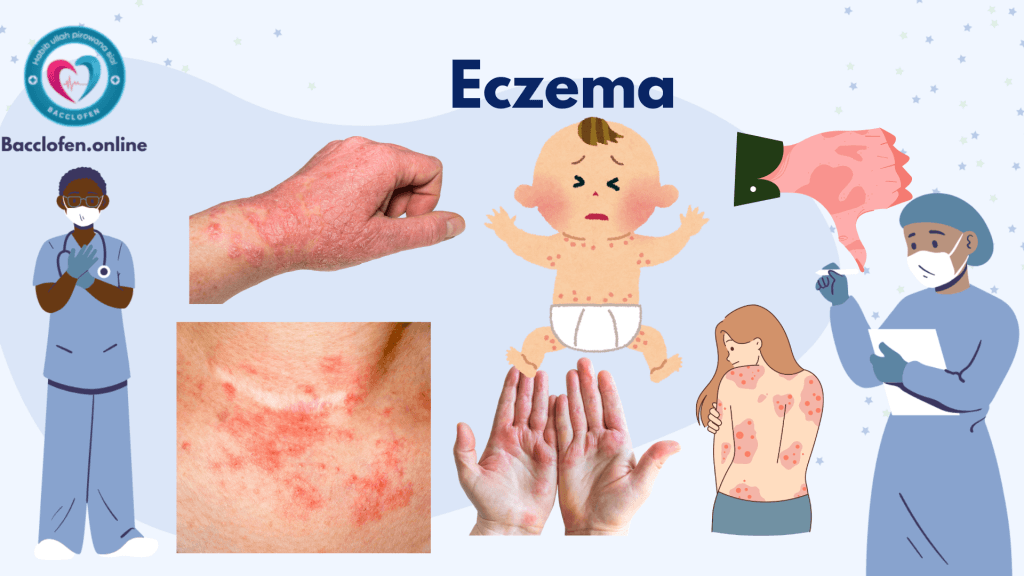
Eczema, also known as atopic dermatitis, is a chronic skin condition characterized by inflammation, redness, itching, and dryness. It is a common condition that can affect people of all ages, though it is most prevalent in children. While eczema is not contagious, it can significantly impact the quality of life due to its persistent and often uncomfortable symptoms. This article explores the causes, symptoms, prevention, diagnosis, and treatment options for eczema.
What is Eczema?
Eczema is an umbrella term for a group of conditions that cause the skin to become inflamed or irritated. The most common form is atopic dermatitis, a condition that often begins in childhood and may persist into adulthood. Other types of eczema include:
- Contact Dermatitis: Triggered by direct contact with irritants or allergens.
- Dyshidrotic Eczema: Characterized by small, itchy blisters on the hands and feet.
- Nummular Eczema: Presents as round, coin-shaped spots on the skin.
- Seborrheic Dermatitis: Affects oily areas of the body, such as the scalp and face.
- Stasis Dermatitis: Occurs in people with poor circulation, typically on the lower legs.
Causes of Eczema
Eczema is thought to result from a combination of genetic, environmental, and immune system factors. These include:
1. Genetic Factors
- A family history of eczema, asthma, or hay fever increases the likelihood of developing eczema.
- Mutations in the filaggrin gene, which is responsible for maintaining the skin’s barrier, can lead to increased susceptibility.
2. Immune System Dysfunction
- Overactive immune responses to irritants or allergens can cause inflammation and skin damage.
3. Environmental Triggers
- Allergens: Pollen, pet dander, mold, or dust mites can exacerbate symptoms.
- Irritants: Soaps, detergents, shampoos, and certain fabrics can irritate sensitive skin.
- Climate: Dry, cold weather or excessive heat and humidity can trigger flare-ups.
4. Lifestyle Factors
- Stress and lack of sleep can worsen eczema symptoms.
- Diet may play a role in some individuals, with foods like dairy, eggs, or nuts potentially triggering flare-ups.
Symptoms of Eczema
Eczema symptoms vary widely and can range from mild to severe. Common signs include:
1. Skin Changes
- Dryness: Skin often feels rough, flaky, and tight.
- Redness and Inflammation: Affected areas become red, swollen, and warm to the touch.
- Itching: Intense itching, which may worsen at night, is a hallmark symptom.
2. Rashes
- Acute Phase: Blisters may ooze and crust over.
- Chronic Phase: Thickened, scaly skin develops due to prolonged scratching (lichenification).
3. Location of Symptoms
- In infants, eczema typically appears on the face, scalp, and extremities.
- In older children and adults, it commonly affects the hands, feet, neck, and areas where the skin folds, such as elbows and knees.
Complications of Eczema
If left untreated or poorly managed, eczema can lead to:
- Skin Infections: Repeated scratching can cause breaks in the skin, allowing bacteria, viruses, or fungi to enter.
- Sleep Disruption: Persistent itching often interferes with sleep quality.
- Emotional Impact: Visible symptoms can lead to self-consciousness, anxiety, or depression.
- Allergic Conditions: Individuals with eczema are more likely to develop asthma or hay fever.
Prevention of Eczema
While eczema cannot always be prevented, the following measures can reduce the risk of flare-ups:
1. Maintain Skin Hydration
- Use fragrance-free, hypoallergenic moisturizers regularly to keep the skin barrier intact.
- Avoid long, hot showers and opt for lukewarm water instead.
2. Avoid Triggers
- Identify and avoid known allergens or irritants, such as harsh soaps or certain fabrics.
- Use mild, fragrance-free detergents and personal care products.
3. Protect the Skin
- Wear gloves while handling cleaning agents or during cold weather to protect the skin.
- Dress in breathable, soft fabrics like cotton to minimize irritation.
4. Manage Stress
- Practice stress-reduction techniques like meditation, yoga, or deep breathing exercises.
Diagnosis of Eczema
A diagnosis of eczema is typically made through:
1. Medical History and Physical Examination
- The doctor will ask about the patient’s symptoms, family history, and possible triggers.
- A visual examination of the affected skin is conducted to assess the condition.
2. Allergy Testing
- Patch or prick tests may be performed to identify potential allergens that could be contributing to eczema.
3. Skin Biopsy
- In rare cases, a small skin sample may be taken to rule out other conditions like psoriasis or fungal infections.
Treatment of Eczema
While there is no cure for eczema, treatments aim to control symptoms, reduce flare-ups, and prevent complications.
1. Topical Treatments
- Moisturizers: Emollients and ointments are essential for hydrating the skin and preventing dryness.
- Corticosteroids: Creams and ointments reduce inflammation and itching during flare-ups.
- Calcineurin Inhibitors: Non-steroidal creams, such as tacrolimus or pimecrolimus, are used for sensitive areas like the face or eyelids.
2. Systemic Treatments
- Oral Medications: Antihistamines can relieve itching, while corticosteroids or immunosuppressants may be prescribed for severe cases.
- Biologics: Newer medications like dupilumab target specific immune pathways and are effective for moderate-to-severe eczema.
3. Phototherapy
- Controlled exposure to ultraviolet (UV) light helps reduce inflammation and improve skin healing.
4. Lifestyle Modifications
- Avoiding known triggers and maintaining a consistent skincare routine can help manage symptoms effectively.
Living with Eczema
Managing eczema requires a comprehensive approach:
- Establish a Skincare Routine: Regular moisturizing and gentle cleansing are essential.
- Monitor Symptoms: Keep a diary to identify potential triggers and patterns.
- Seek Support: Joining support groups or speaking with a therapist can help with the emotional challenges of living with eczema.
Research and Future Directions
Advances in eczema research continue to improve treatment options:
- Genetic Studies: Identifying genetic markers associated with eczema can lead to personalized treatments.
- Targeted Therapies: New biologics and immune-modulating drugs offer hope for individuals with severe eczema.
- Probiotics and Microbiome Research: Exploring the role of gut and skin microbiota in eczema may lead to novel preventive strategies.
Pingback: Acne: Causes, Symptoms, Preventions and Treatment - Bacclofen