Lupus, or systemic lupus erythematosus (SLE), is a chronic autoimmune disease where the body’s immune system mistakenly attacks its own tissues and organs. This leads to inflammation that can affect various systems, including the skin, joints, kidneys, heart, lungs, and brain. Lupus is a complex and often misunderstood disease due to its diverse symptoms and varying severity among individuals. This article provides a comprehensive overview of lupus, focusing on its causes, symptoms, prevention, diagnosis, and treatment.
Causes of Lupus
The exact cause of lupus remains unknown, but it is believed to result from a combination of genetic, environmental, and hormonal factors.
1. Genetic Factors
- Individuals with a family history of lupus or other autoimmune diseases are at an increased risk.
- Certain genes associated with the immune system may predispose individuals to lupus.
2. Environmental Triggers
- Exposure to ultraviolet (UV) light can trigger or worsen lupus symptoms.
- Infections, such as Epstein-Barr virus (EBV), may trigger lupus in genetically susceptible individuals.
- Certain medications, including hydralazine and procainamide, can cause drug-induced lupus, a reversible condition.
3. Hormonal Influence
- Lupus is more common in women, particularly during reproductive years, suggesting a link with female hormones like estrogen.
- Hormonal fluctuations, such as those during pregnancy or menstrual cycles, can influence lupus activity.
Symptoms of Lupus
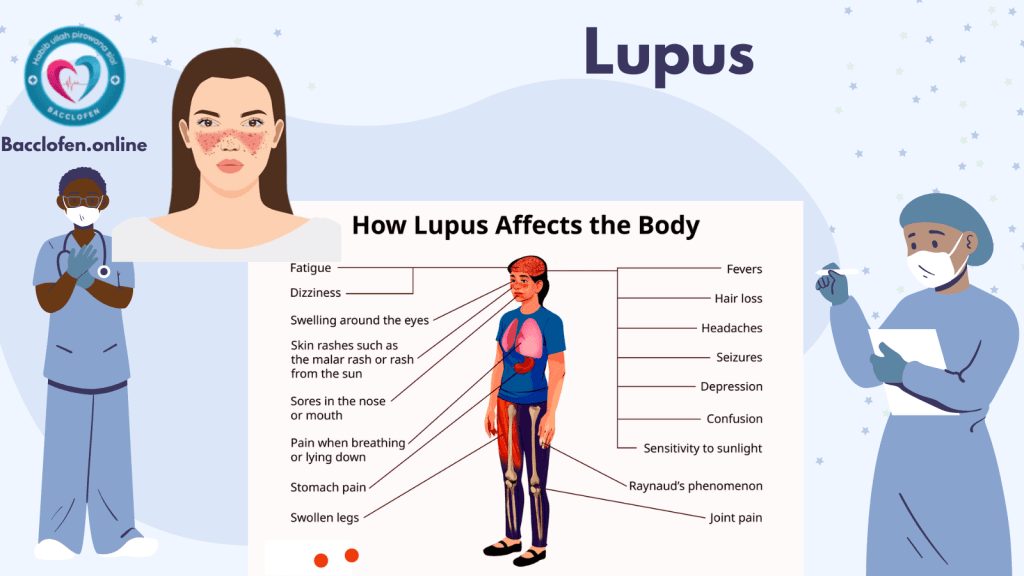
Lupus symptoms vary widely and can mimic those of other conditions, earning it the nickname “the great imitator.” Symptoms can develop gradually or appear suddenly, and they often alternate between periods of flares and remission.
Common Symptoms
- Fatigue: Persistent tiredness is one of the most common symptoms of lupus.
- Joint Pain and Swelling: Often affects the hands, knees, and wrists.
- Skin Rash:
- The “butterfly rash” across the cheeks and nose is a hallmark sign.
- Other rashes may appear on sun-exposed areas.
- Fever: Low-grade fever without an apparent cause.
- Photosensitivity: Sensitivity to sunlight can exacerbate rashes and other symptoms.
Systemic Symptoms
- Kidney Issues (Lupus Nephritis): Swelling in the legs or around the eyes, and foamy urine due to protein leakage.
- Cardiovascular Problems: Inflammation of the heart (pericarditis) or blood vessels.
- Respiratory Issues: Shortness of breath due to pleuritis or lung inflammation.
- Neurological Symptoms: Headaches, confusion, seizures, or memory loss.
Complications of Lupus
Lupus can cause damage to various organs and systems, leading to severe complications:
- Kidney Failure: Lupus nephritis is a major cause of mortality in lupus patients.
- Cardiovascular Disease: Lupus increases the risk of heart attacks, strokes, and hypertension.
- Infections: Immunosuppression from lupus or its treatments can make patients more susceptible to infections.
- Blood Disorders: Anemia, low platelet count, or blood clot formation (antiphospholipid syndrome).
Prevention of Lupus
Since lupus is not entirely preventable, the focus lies on minimizing triggers and managing risk factors.
1. Avoid Sun Exposure
- Use broad-spectrum sunscreen and wear protective clothing to reduce UV-related flares.
2. Manage Stress
- Practice relaxation techniques like meditation or yoga to reduce stress-induced flares.
3. Limit Exposure to Infections
- Practice good hygiene and stay up-to-date with vaccinations (consult a doctor, as live vaccines may not be suitable).
4. Monitor Medications
- Discuss medications with a healthcare provider to avoid those that may trigger drug-induced lupus.
Diagnosis of Lupus
Diagnosing lupus is challenging due to its diverse symptoms. No single test can confirm lupus; instead, a combination of clinical evaluation and laboratory tests is used.
1. Medical History and Physical Examination
- A detailed history of symptoms and family medical history is crucial.
- A physical exam assesses rashes, joint swelling, and other visible signs of lupus.
2. Laboratory Tests
- Antinuclear Antibody (ANA) Test: A positive ANA test suggests an autoimmune condition.
- Anti-dsDNA and Anti-Smith Antibodies: Specific markers for lupus.
- Complete Blood Count (CBC): Detects anemia, low white blood cell, or platelet counts.
- Urinalysis: Checks for protein or blood in urine, indicative of kidney involvement.
3. Imaging and Biopsies
- Chest X-rays and Echocardiograms: Evaluate lung and heart involvement.
- Kidney Biopsy: Confirms lupus nephritis and guides treatment.
Treatment of Lupus
While there is no cure for lupus, treatment aims to manage symptoms, prevent flares, and reduce organ damage.
1. Medications
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs): Relieve pain and inflammation.
- Antimalarials: Hydroxychloroquine is commonly used to control skin and joint symptoms and prevent flares.
- Corticosteroids: Used to control inflammation in severe cases, but long-term use has side effects.
- Immunosuppressants: Medications like azathioprine, mycophenolate mofetil, or cyclophosphamide are used for severe organ involvement.
- Biologics: Belimumab is a targeted therapy for lupus.
2. Lifestyle Changes
- Maintain a healthy diet rich in anti-inflammatory foods, like fruits, vegetables, and omega-3 fatty acids.
- Exercise regularly to improve overall health and reduce fatigue.
- Adequate rest to combat fatigue and stress.
3. Regular Monitoring
- Routine check-ups to monitor disease activity and medication side effects.
- Regular kidney function and blood pressure assessments for early detection of complications.
Living with Lupus
Living with lupus requires a proactive approach to health and wellness. Support systems, including healthcare providers, family, and patient groups, play a crucial role in improving the quality of life.
Self-Care Tips
- Adhere to Treatment Plans: Follow prescribed medications and attend regular medical appointments.
- Educate Yourself: Learn about lupus to recognize warning signs of flares.
- Seek Support: Join lupus support groups for emotional and practical advice.
Research and Future Directions
Ongoing research is focused on understanding the mechanisms of lupus and developing targeted therapies. Areas of interest include:
- Genetic Studies: Identifying genes associated with lupus to understand its hereditary nature.
- Biologic Therapies: Exploring new biologics that selectively target immune pathways.
- Precision Medicine: Tailoring treatments based on individual genetic and clinical profiles.
Also check
Pingback: Malnutrition: Causes, Symptoms and Treatment - Bacclofen