Psoriasis is a chronic autoimmune condition that primarily affects the skin, causing red, scaly patches. While it can occur at any age, psoriasis typically develops in early adulthood or later in life. This non-contagious condition varies in severity, ranging from small, localized patches to widespread plaques. Although there is no cure for psoriasis, effective treatments and lifestyle adjustments can significantly manage symptoms and improve quality of life.
This article provides a detailed overview of psoriasis, discussing its causes, symptoms, prevention, diagnosis, and treatment options.
What is Psoriasis?
Psoriasis is an autoimmune disorder where the immune system mistakenly accelerates the life cycle of skin cells, causing them to build up rapidly on the surface. This results in inflamed, thickened patches of skin covered with silvery scales. Psoriasis is not merely a skin condition; it can also lead to systemic complications, including psoriatic arthritis, which affects the joints.
Causes of Psoriasis
The exact cause of psoriasis is unknown, but it is believed to result from a combination of genetic, immune, and environmental factors.
1. Genetic Factors
- Psoriasis has a strong hereditary component. If one or both parents have psoriasis, the risk of developing the condition increases significantly.
- Specific gene mutations are linked to psoriasis, particularly those affecting immune system regulation.
2. Immune System Dysfunction
- Psoriasis is an autoimmune condition where the immune system attacks healthy skin cells.
- T-cells, a type of white blood cell, mistakenly trigger an inflammatory response, causing rapid skin cell production.
3. Environmental Triggers
- Certain triggers can exacerbate or initiate psoriasis, including:
- Stress: Emotional or physical stress can trigger flare-ups.
- Infections: Strep throat and skin infections are common triggers.
- Injury to Skin: Cuts, burns, or insect bites can lead to psoriasis at the injury site (Koebner phenomenon).
- Medications: Drugs like beta-blockers, lithium, and antimalarial medications can provoke symptoms.
- Lifestyle Factors: Smoking, excessive alcohol consumption, and obesity are associated with psoriasis onset and severity.

Symptoms of Psoriasis
Psoriasis symptoms vary depending on the type and severity. Common signs include:
1. Plaque Psoriasis
- The most common form, characterized by raised, inflamed patches of skin covered with silvery-white scales.
- Often appears on the scalp, elbows, knees, and lower back.
2. Guttate Psoriasis
- Small, drop-shaped sores often triggered by infections.
- Common in children and young adults.
3. Inverse Psoriasis
- Red, shiny lesions in skin folds, such as under the breasts or around the groin.
- Worsened by friction and sweating.
4. Pustular Psoriasis
- White pustules surrounded by inflamed skin.
- Can be localized to the hands and feet or more widespread.
5. Erythrodermic Psoriasis
- A severe, rare form causing widespread redness, shedding of skin, and intense pain.
- Often triggered by untreated psoriasis or withdrawal from systemic treatments.
Other Symptoms
- Itching, burning, and discomfort in affected areas.
- Thickened or ridged nails, sometimes leading to nail separation (onycholysis).
- Joint pain and swelling in cases of psoriatic arthritis.
Complications of Psoriasis
Without proper management, psoriasis can lead to several complications, such as:
- Psoriatic Arthritis: A painful inflammatory condition affecting joints.
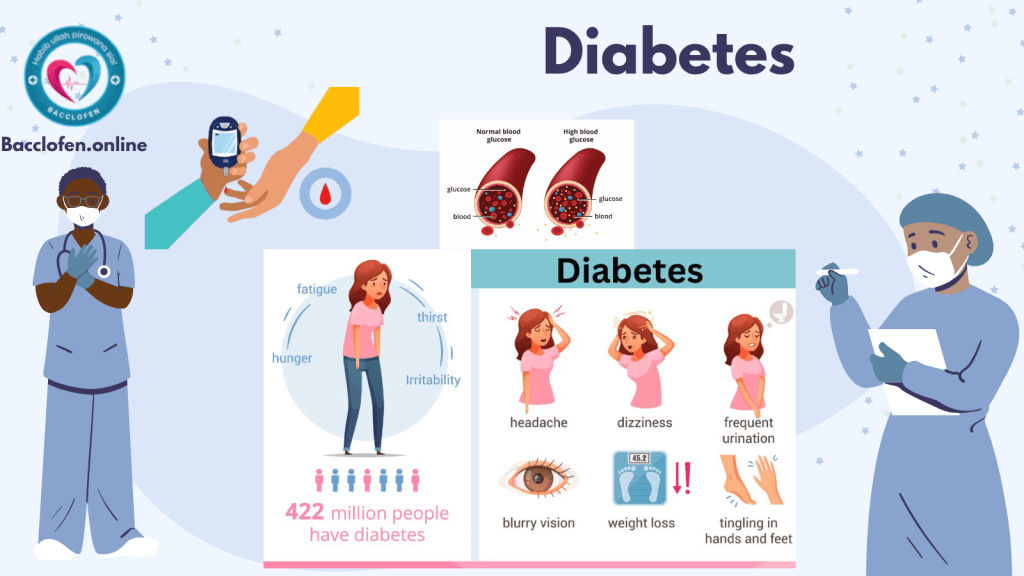
- Increased Risk of Other Conditions: Psoriasis is linked to a higher risk of cardiovascular disease, diabetes, and depression.
- Emotional and Social Impact: Visible lesions can lead to self-esteem issues and social isolation.
Prevention of Psoriasis
While psoriasis cannot be entirely prevented, certain strategies can help reduce the frequency and severity of flare-ups:
1. Manage Triggers
- Avoid known triggers, such as certain medications or stressors.
- Protect the skin from injuries and infections.
2. Maintain a Healthy Lifestyle
- Quit smoking and limit alcohol intake, as both are known to worsen symptoms.
- Follow a balanced diet rich in anti-inflammatory foods like fruits, vegetables, and omega-3 fatty acids.
3. Manage Stress
- Engage in relaxation techniques, such as meditation, yoga, or deep breathing exercises, to reduce stress-induced flare-ups.
4. Hydrate Skin
- Use moisturizers regularly to prevent dryness and cracking.
Diagnosis of Psoriasis
Psoriasis is diagnosed based on clinical evaluation and sometimes additional tests:
1. Physical Examination
- A dermatologist examines the skin, nails, and scalp for typical signs of psoriasis.
- A detailed medical history, including family history, is reviewed.
2. Skin Biopsy
- In uncertain cases, a small skin sample may be taken and analyzed under a microscope to confirm the diagnosis.
3. Blood Tests
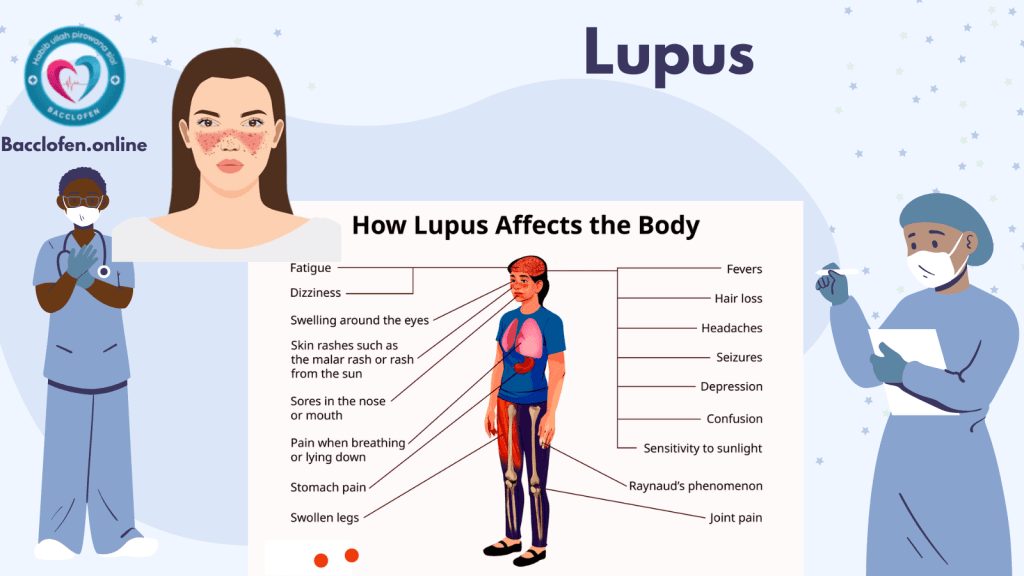
- May be conducted to rule out other conditions with similar symptoms, such as lupus or eczema.
Treatment of Psoriasis
Psoriasis treatment focuses on controlling symptoms, reducing inflammation, and slowing skin cell growth. Options include:
1. Topical Treatments
- Corticosteroids: Reduce inflammation and slow skin cell turnover.
- Vitamin D Analogues: Calcipotriol helps to slow skin cell production.
- Coal Tar: Eases scaling, itching, and inflammation.
- Salicylic Acid: Removes scales and promotes smoother skin.
2. Phototherapy
- Involves exposing the skin to controlled amounts of natural or artificial ultraviolet (UV) light.
- UVB therapy and PUVA (psoralen plus UVA) are common methods.
3. Systemic Medications
For moderate to severe cases, medications that affect the entire body are used:
- Methotrexate: Slows skin cell production and suppresses the immune system.
- Cyclosporine: Reduces immune system activity.
- Biologics: Target specific parts of the immune system (e.g., TNF-alpha inhibitors like adalimumab or IL-17 inhibitors like secukinumab).
4. Lifestyle Adjustments
- Regular exercise to reduce inflammation.
- Stress management techniques to prevent flare-ups.
5. Alternative Therapies
- Certain natural remedies, such as aloe vera or omega-3 supplements, may provide symptom relief.
Living with Psoriasis
Managing psoriasis requires ongoing effort and support. Here are some strategies to enhance quality of life:
1. Build a Support Network
- Joining psoriasis support groups can help share experiences and find encouragement.
2. Regular Check-Ups
- Monitor symptoms and adjust treatment as needed.
3. Educate Yourself
- Stay informed about the condition and new treatment options.
Research and Future Directions
Research on psoriasis is focused on developing more effective and less invasive treatments, including:
- Advanced Biologics: New biologics with fewer side effects and better efficacy.
- Gene Therapy: Potential to target and correct genetic predispositions.
- Personalized Medicine: Tailoring treatments based on individual genetic and immune profiles.
Pingback: Menstrual disorders: Types, Causes, Symptoms and Risk factors - Bacclofen